Why Diet Matters in Chronic Disease.
How do nutrient deficiencies contribute to our epidemic of chronic diseases?
Nutrition is not a straightforward subject. The confusion over how best to obtain health is played out amid the ‘diet wars’, which refer to the ongoing debates and hostility between conflicting diet and nutrition approaches. Media headlines continue to contribute to our misunderstandings by reporting what is healthy one day, only to deem it ill-advised the next. Social media is another major driver of our healthy living culture, as professionals and influencers compete in promoting various diet and lifestyle trends. However, as our exposure to wellness information increases, contradictions are inevitably found, putting many health-conscious individuals at risk of misleading content or increasing their disillusionment with what truly works.
Furthermore, you might believe that diet is too inconsequential to be considered a key factor in the development of chronic illness or that its effects are too limited to be emphasised in the treatment of disease. It is certainly what I thought at the start of my own health struggles. I didn’t eat that badly, so how could my diet be to blame for my suffering, I thought? The symptoms I had experienced were serious and longstanding, not something minor brought on by a lack of vitamins. However, after much trial and error with several healing modalities, I ultimately concluded that nutrition was what mattered most, and if I didn’t find the right way of eating, my health would continue to deteriorate.
Nutrients are the raw materials that enable the physiological and psychological chemical processes, which govern our behaviour, thoughts, and emotions. Every bodily reaction involves communication via interdependent electrical and chemical signals. It’s impossible to grasp its complexity; humans are made up of a mass of trillions of cells, and each cell is estimated to perform about a billion biochemical reactions per second.
Life itself depends upon these chemical changes, which regulate the digestion of food into smaller components that facilitate energy production, enabling movement and proper functioning of the nervous system and brain. When these processes are disrupted in any way, we refer to it as disequilibrium, where the shift in the body’s homeostasis leads to adverse symptoms. As these chemical processes are dependent on the production and use of enzymes supplied by vitamins, the very first step in reversing symptoms is to ensure optimal nutrient status. (2)(4)
Although we may be aware of what needs correcting, finding the right nutrition programme to facilitate these changes can prove challenging. The generic health recommendations I had received and read about were not appropriate for my illness or, as it happens, most chronic disorders. It wasn’t until I came across a book titled “Gut and Psychology Syndrome” that I could begin the healing process and gain elucidation as to why everything I had previously tried had failed. One of the main reasons for my lack of success with other regimens was not that nutrition is insignificant in health restoration, but rather that there can only be one way to address the nutritional needs of a diseased body.
GAPS taught me something unique to other protocols: that the health of the digestive system is fundamental in the initiation and progression of chronic diseases. And until its function improves, nutrient malabsorption will persist, and so too will the dysfunctionality of the immune system. This realisation made perfect sense to me. As my digestion was under strain, I had to eat in a way that allowed maximum nutrient absorption while also not aggravating the damage already done. The GAPS diet was unconventional and not common knowledge, yet there was no paucity of evidence supporting its usefulness. So why had I not heard of it? (5)
Getting Back To Basics.
What appears to have been lost in nutrition science and education is the fundamental reason why we eat. It may be surprising to learn, but some of the most commonly recommended diets are actually the most difficult for us to digest and absorb nutrients from. We all understand that nutrients are essential for sustaining life, but with access to an abundance of food, few of us concern ourselves with the idea of insufficient nourishment. However, the assurance of food surplus in nutritional maintenance is based on a false equivalence. We are living through a period of dramatic environmental change that is unlike any other in human history. Modern industrialisation, particularly since the third industrial revolution post-World War II, has led to significant transitions in how we manufacture and produce. Additionally, these advancements have led to the exponential rise in the number and quantity of commercially available chemicals. (1)(5)
Hundreds of thousands of inadequately tested chemicals enter circulation each year, polluting our environment and bodies and raising our risk of disease. In recent decades, technology and the agrochemical industry have transformed agriculture through intensive farming practices that support large-scale crop production and spraying, leading to a decline in the quality and nutrient profile of our diets. Furthermore, food manufacturers have devised new methods for producing ultra-processed foods that no longer resemble natural food products, as they are increasingly laden with synthetic ingredients that replace essential nutrients. Consequently, as our diets become more processed, often due to rising food costs, the risk of developing nutrient deficiencies remains a significant public health concern. (1)(4)(5)
Therefore, given our modern reality, dietary advice should be pretty straightforward: nutrients confer health, and the diet that best meets our nutritional needs is the one we should follow. However, nutrition remains a complicated and contentious subject for academics and laypeople alike, and this basic concept of health does not seem so evident to all. To unravel our modern health conundrum and establish what we should eat, we first need to revisit the basics of nutrition.
Deficiency Disorders From The Past and Present.
Below is a short summary of some of the most severe deficiency disorders that once plagued various populations around the world.
Between the 1600s and 1800s, it is estimated that about 1,000,000 sailors died at sea from scurvy, a disease caused by a serious vitamin C deficiency. Ascorbic acid (vitamin C) is essential for collagen synthesis, the body's most abundant protein, and its deficiency leads to degeneration of connective tissues, including cartilage, bone, skin, and muscles. Untreated scurvy is invariably fatal. (3)(4)
A prolonged vitamin D deficiency gives rise to the bone condition rickets. Historically, this condition was prominent in 17th-century London, where thick smog resulting from the city’s coal-burning industry was thought to have prevented adequate sunlight exposure, leading to abnormal development in many children. (3)(4)
Deficiency in niacin (vitamin B3) causes pellagra, a condition characterised by the four Ds: diarrhoea, dermatitis, dementia, and death. The condition was first identified in the 1700s, but rose to prominence during the early 20th century among South American populations consuming a maize-based diet. Old attitudes biased medics who had observed similar symptoms in tropical diseases, and confused authorities denied that pellagra was not a contagious illness. Eventually, after many drastic experiments, it was proven that pellagra did not occur in those consuming nutrient-dense diets of meat and dairy.
Retinol (vitamin A) deficiency is consistently reported to be among the most common nutrient deficiencies in both developing and developed nations. A serious lack of vitamin A is the leading cause of preventable blindness in children, but it also adversely affects gut microbial composition, while compromising immune and gastrointestinal health. According to some research, all chronic liver diseases are associated with vitamin A deficiency. (3)
A severe form of thiamin (vitamin B1) deficiency, known as beriberi, was reportedly the primary cause of Asian morbidity and mortality from the 1600s to the early 1900s. The main feature of this disease was oedema and paralysis of the lower limbs. It was described by an Asian medical board in 1832 as being “insidious in its attack, rapid in its progress, and fatal in its termination.” Milled rice exports to Asia became the principal, and in some populations, the exclusive diet of certain social groups. With so many political and commercial interests at stake, it took centuries for the disorder to receive its deserved recognition.
A beri-beri patient. https://en.wikipedia.org/wiki/Thiamine_deficiency
These disorders are prime examples of how history has taught us little about the devastation micronutrient deficiencies have caused humanity. Their aftermath rivalled those of the common communicable epidemics of that era, yet by the early 20th century, nutritional causes of diseases were already considered “anachronistic” (old-fashioned), and dismissive and aloof attitudes persisted regarding the threat they posed. Until this point, scientific research had concentrated on the origins of infectious diseases, and with medicine entrusted with discovering cures for pathogens, the field gained a level of glamour and prestige that overshadowed other disciplines. As nutritional research gradually evolved into an established science, competing medical communities disputed claims of deficiency syndromes and remained stubbornly unperturbed by their gravity. As a result, efforts to inform the public were slow, inadequate, and often too late.
What Has Gone Wrong In Chronic Disease?
Micronutrient is an umbrella term used to represent essential dietary vitamins and minerals required to sustain virtually all normal cellular and molecular functions. Single micronutrient deficiencies (MNDs) rarely happen in isolation, and more often, multiple MNDs co-occur. The most common nutrient deficiencies are vitamin A, folate, zinc, iodine, and iron. However, several other deficiencies are prevalent, including B12, vitamin D, selenium, magnesium, and calcium. We only need vitamins in very small amounts, yet MNDs are widespread across the developed world. Reports that aim to ameliorate such trends tend to focus on insufficient dietary intake, particularly one that is low in fruits and vegetables. The irony is that neither food choice is a good source of the most common nutrient deficiencies, nor have they been in the past. Although limited and processed diets were once the cause of deficiency disorders, and this fact still holds true today, there are now other risk factors to contend with. (4)(3)
Food variety does not always equate to nutritional diversification. Another consequence of reduced food quality and chemical contamination is impaired nutrient absorption due to inflammation and disease. As mentioned previously, the GAPS person cannot follow conventional wisdom by consuming a "well-balanced diet" because the disease originates in the gut, and the digestive system is now too damaged by man-made products to digest certain foods properly. Biocides, such as insecticides and pesticides, are potent poisons that not only eradicate environmental pests and damage the microflora of the soil but also harm the living bacteria residing in our guts. In cases of debility involving autoimmunity or neuropsychiatric illness, merely avoiding processed foods is insufficient to optimise our biochemistry and reverse disease. (1)(5)
The core issue to address in disease states is dysbiosis, the imbalance of microbial communities within the body and their migration. A healthy microbiome is crucial for the digestive system to synthesise and absorb nutrients, and unless the gut flora is modulated in a way that allows it to achieve a healthy diversity, nutritional status will remain inadequate. (1)(5)
Components of the mucosal barrier, such as the growth of epithelial cells (cells that facilitate nutrient absorption), will weaken, and their renewal is inhibited if digestion is impaired. Undigested food particles become food for pathogenic microorganisms, and toxic microbial metabolites further damage the intestinal tract, preventing complete assimilation. The permeable gut enables these toxic compounds, heavy metals and other environmental substances to enter the body and access the brain. This continual flow of bacteria and external pollutants into the bloodstream establishes our disease state by inducing the activation of immunological complexes, such as inflammatory cytokines, which also heighten our susceptibility to complications. (2)(5)
For this reason, consuming many mainstream health foods and 'superfoods' — such as those shown in the picture above — is not suitable for individuals with pathological gut permeability and pathogenic overgrowth. In fact, most commensal microorganisms harboured by microbial ecosystems are pathobionts; that is, in conditions of imbalance and immunosuppression, they can act as pathogens. This is why the forms of nutrients that differ between plant and animal varieties, as well as their molecular structures, chemical compounds, and fibrous content, all need to be considered when attempting to modify the gut environment. Consequently, only easily digestible, nutrient-dense foods that do not stimulate microbial growth should be initially encouraged.
GAPS' unique approach is not about demonising certain foods, as some may think, but about understanding that the biological conditions in those who are sick are very different from those of healthy individuals. Current food-based dietary guidelines are not yet microbiome-oriented in a way that reverses disease but generally provide recommendations for health maintenance. It has long been demonstrated, however, that microbially produced metabolites from dietary sources regulate immunity, endocrine, and nervous system functions, supporting their causal role in various health domains. As such, certain unorthodox measures are necessary to restore normal physiology and intestinal immunity. (1)
The Global Burden of Micronutrient Deficiencies.
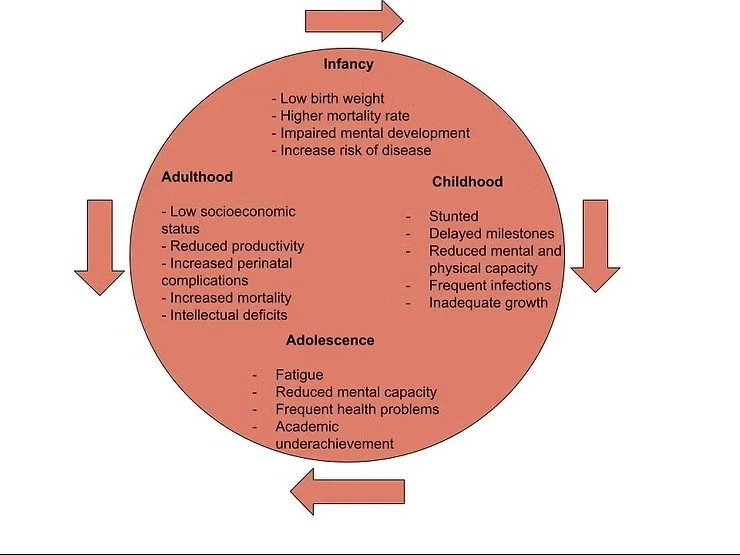
Nutrition is not something we can afford to take lightly. Micronutrient deficiencies (MNDs) have a direct and lasting impact on individuals and societies. Poorer health, premature death, personality changes, academic underachievement, reduced work capacity, and lower earning potential are all direct consequences of undernutrition. What compounds these concerns is the heritability cycle of MNDs that perpetuates across generations. Malnutrition not only has detrimental effects on individuals and families but also generates vast social and economic downfalls, including a propensity towards financial dependency, higher criminality, and addictive tendencies.
The Intergenerational Cycle of Micronutrient Deficiency.
Poverty is indeed the greatest predictor of MNDs, and low- and middle-income countries bear the highest burdens. However, high-income countries are witnessing high illiteracy rates, and behavioural control and socialisation problems are steadily increasing among school-aged children. Westernised societies are witnessing sharp mental health deterioration and plummeting infertility rates, while obesity, autoimmunity, and other chronic diseases have reached epidemic proportions. Suboptimal nutritional status can have particularly far-reaching and enduring implications when it occurs in utero or during early childhood development. It is also possible that epigenetic marks (modifications to DNA) acquired by prior generations through environmental insults are passed down, increasing our susceptibility to the health defects of our parents. As the old saying goes, “The apple doesn’t fall far from the tree!” (1)(5)
The resulting mental and physical impairments may begin as mild issues during childhood, such as frequent infections or allergies that are dismissed as normal occurrences, or increased anxiety or impulsivity explained as unique personality traits. Many serious health effects may only become apparent during puberty, as hormone shifts intensify the consequences of abnormal biochemistry. These events represent a spectrum of diseases that can predispose a child to a cascade of circumstances that appear unrelated, but alter the entire life course. Although certain diagnoses have increased in parts of the world, most children and adolescents will never be diagnosed with any disorder, much less one that is accurate. (5)
Nutritional deficiencies contribute to disease by potentially altering DNA methylation, an essential epigenetic determinant of gene expression that regulates gene activity, maintains DNA integrity, and modulates mutations. The microbiome also plays a significant role in genetic expression, influencing how genes are turned "on" and "off". Several nutritional deficiencies are involved in the enhanced absorption of toxic metals such as cadmium. Metal toxicity is another risk factor in the pathogenesis of mental disorders, which have been extensively researched for their deleterious effects on the brain and nervous system. Key nutrients also maximise the effectiveness of detoxification, including heavy metal metabolism, facilitated mainly by zinc-dependent proteins (1) (2).
"Nutrients are the raw materials used to synthesise neurotransmitters that are continuously produced in the brain and may be at improper concentrations when inadequate nutrition is supplied." - Walsh, 2014.
Undernutrition is the leading cause of immunodeficiency worldwide, and the most common MND deficiency is iron, affecting more than 30% of the world's population. Iron supplementation has experienced one of the greatest growths in popularity in recent years, as the prevalence of iron deficiency anemia continues to rise. Low iron stores disrupt the optimal function of both the endocrine and immune systems, and it is a particularly common deficiency during pregnancy, in which it is associated with many perinatal complications. Iron is critically important for growth and cognitive function and is a necessary component of hemoglobin, which is needed for oxygen transport and cellular respiration.
However, dietary guidelines and nutritionists often fail to differentiate between the two types of iron that exist: heme iron from animal products and non-heme iron found in plants. Heme iron is more bioavailable, estimated to be 12-25%, and non-heme iron has less than 5% bioavailability. Another factor that inhibits iron absorption from food is plant antinutrient compounds, including phytates and lignins, which function as mineral chelators, as well as fibre that reduces mineral absorption. In conjunction with damaged gut flora, the emphasis on plant consumption over animal products further reinforces the risk of many nutrient deficiencies. (5)
Dietary Supplements, and the Interaction Between Diet, Environment, and Gut Microbiome.
The role of the clinician is imperative in recognising and interpreting the biomarkers of micronutrient deficiencies. However, standard blood test results are often deemed "normal" despite a patient presenting with a list of health complaints. Without an identifiable cause, patient symptoms are minimised, and reassurance is given that there is nothing wrong. Unfortunately, many biological measurements are non-specific (i.e. blood, urine) and are not available for all biochemicals, with other biomarkers influenced by confounding variables such as infection or inflammation. However, a chronically ill person likely suffers from the culmination of undernutrition and lack of antioxidant protection, which has failed to defend the body against chemical hazards and subsequent disease. Parallels can be drawn between deficiency disorders of the past and today's management of chronic illnesses. The insurmountable number of environmental stimuli to which modern humans are exposed is now of the greatest relevance in disease incidence, yet mainstream medicine has failed to attribute the escalation to anything out of the ordinary. (1)
"The warning signs of chemical exposures are not posted on office or bathroom walls; they are not even listed on the containers that hold the chemicals. For the most part, evidence of the existence of these chemicals and their potential damage to our health and that of future generations lies buried in the annals of academic libraries." - Integrative Environmental Medicine (2).
Along with nutritional deficiencies, severe oxidative stress is another distinctive feature of chronic illness, as nutrients serve as antioxidants and cofactors for the endogenous production of these compounds. However, antioxidant therapies in the form of nutritional supplements are not always the most effective way to alleviate symptoms and may even exacerbate them. Although taking supplements may seem like a tempting and convenient way to address underlying issues, they are not a replacement for lifestyle changes, which will always yield greater long-term benefits than relying on too many healing agents. Healing happens in stages, and trying to expedite the body's detoxification and regenerative capacity beyond its readiness can spell much frustration with potential setbacks. Antioxidant activity is more complex than simply having enough; what we do know is that most antioxidants can behave as prooxidants under certain conditions — it all depends on the concentration and neighbouring molecules within the body. Again, the environment is everything in determining functionality. (2)
Contrary to the above, functional medicine practitioners usually advise differently. Typically, when a client presents with a chronic disease, a slew of nutritional supplements and antioxidant support is included in the treatment plan. NAC, omega-3 fatty acids, probiotics, herbs, anti-fungal treatments, protein powders, and a range of vitamins and minerals are suggested to improve abnormal biomarkers. Supplemental amino acids are particularly troublesome, as they serve as precursors to neurotransmitters, and considerable trial and error is involved in their use. For example, the amino acid glutamine is frequently recommended to aid recovery, as it is the primary fuel for intestinal cells. However, glutamine is converted into the brain's main excitatory neurotransmitter, glutamate. Evidence indicates glutamatergic dysfunction plays a vital role in the development of many major psychiatric disorders, where glutamine levels have been found to positively correlate with the severity of psychotic symptoms.
Nutritional supplementation, therefore, is not a straightforward process. It is worth noting that there are growing concerns that supplemental nutrients may exhibit different physiological responses and absorption than nutrients found in food. Although they prevent the most dramatic effects of severe nutrient deficiency, they can also initiate adverse reactions that may impede making a full recovery.
An incompetent intestinal and blood-brain barrier makes an individual highly sensitive to the ingestion of many ingredients. Most clients complain that they cannot "eat anything" without a reaction and already avoid certain foods. If left untreated, this situation usually results in the gradual development of new intolerances and sensitivities. The recommended diet will still be limited, but it will contain all the essential nutrients needed to heal, eventually allowing the individual to enjoy a greater variety of foods in the future. However, the constant toing and froing between foods will remain if a person removes only some offending foods but continues to consume others that contribute to the damage of biological membranes. This risk is also true of supplements. Fillers, additives, preservatives, and emulsifiers contained in tablets and capsules have the potential to irritate the delicate intestinal lining and stimulate immune responses. (5)
It is therefore imperative that lifestyle changes are realised as foundational to the normalisation of metabolic activities and the correction of brain chemistry. Nutritional supplements do have the potential to ameliorate symptoms in patients with various disorders, including digestive abnormalities. However, biochemical deficiencies often result from deeper metabolic issues that, as Dr Ruscio warns, “occur secondary to gut dysfunction”, and as such, their use is limited. GAPS disorders require the gut flora composition to shift naturally through the inclusion of antioxidant-rich, nutrient-dense foods, which will initially reduce the likelihood of complications from remedies that can be introduced later, depending on one’s progress.
Researchers increasingly postulate that, for many chronic conditions—from obesity to diabetes, cardiovascular disease to autism and schizophrenia—the interplay between the gut microbiome and various pathways—including the endocrine, nervous, metabolic, and immune systems—plays a central role in the development of disease states. In fact, more scientists agree that no conversation on genetics and health is complete without discussing the function of the microbiome. The gut microbiome interacts with the genome (the complete set of genetic information within an organism) and epigenome, and all of these factors are modulated by diet, nutrition, and the environment. Since intestinal permeability and dysbiosis are at the root cause of many diseases, understanding what constitutes an appropriate diet is key to disease prevention and health restoration (1)
References:
Cohen A, Saal F. Integrative Environmental Medicine. United States: Oxford University Press; 2017.
2. Walsh, W. Nutrient Power. Heal Your Biochemistry And Heal Your Brain. 2nd Edition. United States: Skyhorse Publishing; 2014.
3. Bender D. Introduction To Nutrition And Metabolism. 3rd Edition. United States and Canada: Taylor and Francis; 2002.
4. Meryn L. Causes and Prevention of Vitamin Deficiency. Britain: Amberwood Publishing; 1995.
5. McBride-Campbell N. Gut and Physiology Syndrome. United Kingdom: Mediform Publishing; 2020.